My Cat Allergy Is Killing Me, But Cupcake Stays (#GotBitcoin)
Pet lovers endure runny noses, watery eyes, rashes and difficulty breathing to keep their animals close; ‘there are no boundaries’. My Cat Allergy Is Killing Me, But Cupcake Stays (#GotBitcoin)

When Olivia Lanes’s allergy test came back positive for cats and dogs, she did what any dedicated pet owner would do. She ignored the results.

Now the 26-year-old graduate student in Pittsburgh is often congested and sneezing. To make matters worse, her cat Cupcake, her other cat Sophie and her dog Nova sleep in her bed right next to her face.
Despite the discomfort, she is thinking about getting another dog. “It’s going to happen at some point,” she says.
It’s no secret that Americans are committed to their animals, but it turns out that some people are taking their devotion even further by willingly suffering for them.
Those pet owners are dealing with watery eyes, runny noses, swollen faces, rashes and difficulty breathing. All the while, their pets appear largely oblivious to their misery.

Tracy Spiering says she has a severe allergy to cat saliva, but Oatmeal Cookie, who is 20 years old, sleeps on her chest at night and sometimes grooms herself right there. “It’s like she knows when I’m having an extra sensitive day,” she says. “There are no boundaries.”
Every other Thursday afternoon, the 49-year-old bookkeeper drives to a doctor in downtown Pittsburgh, where she gets three shots in her arm. She sits for 20 minutes in the waiting room to ensure her body doesn’t overreact to the treatment.
If she were to return home to her three cats without the shots, she would be congested, with a runny nose and itchy eyes. Getting rid of them, she says, isn’t an option.
“They are like my children,” says Ms. Spiering, who has an adult daughter. “It would be like giving away your kid.”
More Americans are reporting symptoms of allergies and asthma. For allergy sufferers, the best course of action is to avoid the trigger, says Kenneth Mendez, chief executive of the nonprofit Asthma and Allergy Foundation of America. “If you have allergies to animals, you really shouldn’t have them around.”
For those unwilling to part ways, he advises they at least keep pets out of the bedroom, avoid carpets in the home and use products certified as asthma and allergy friendly.

Olivia Johnson, 22, says her allergy to dogs, however, is so severe that even with a humidifier, an air purifier, multiple doctor visits, prescription medication, a nasal spray and an inhaler, the symptoms are still there.
The day Ms. Johnson brought home her German shepherd, Avery, she developed itchy skin, tightness in her chest and difficulty breathing. Three years later, the symptoms haven’t gone away. “It’s constant,” says the waitress who lives in Denver. “I feel awful.”
Some people seek out “hypoallergenic” dogs or hairless cats, which are supposed to spread fewer allergens. Mr. Mendez says such claims are unproven. “There’s no such thing as a hypoallergenic animal,” he says.
The American Kennel Club lists hypoallerengic dogs on its website, although it cautions that no dogs are 100% so. “We encourage people to interact with the breed, and also the specific dog they are interested in, to see if they have a reaction,” says an AKC spokeswoman.
Some desperate pet owners have turned to remedies such as antiallergen dog shampoo, carpet deodorizer and face masks.
Camryn Bourne, a 13-year-old whose pet hedgehog, Lysander, makes her hands swell, has been using a towel to create a physical barrier between herself and the small spiny mammal. The Dallas resident says she relies on her 12-year-old sister to bathe the animal.

Ashok Wahi, a 69-year-old Basking Ridge, N.J., resident, says he invented an over-the-counter gel that functions like a filter for the nose to help his daughter, who was 8 at the time, tolerate her cat Ebony.
The $14.85 product called NasalGuard, which is sold online, claims to “create an invisible filter around the outside of your nasal passages.” Mr. Wahi says he has sold over 12 million tubes since he created the gel in the 1990s.
Patients usually know they are allergic to their pets before showing up for an allergy test, says Eric Caplan, a board-certified allergy specialist in Colorado Springs, Colo. “They have a gut instinct, and it’s usually correct.”

Dr. Caplan says he pushes owners to find a new home for pets if they have severe asthma. In those cases, patients can end up in the emergency room during a flare-up, he says. But even then, some patients refuse to say goodbye.
Susan Cosby has spent years championing cats, whose presence makes her sick. She says she was able to begin working at a pet shelter, even though such facilities usually don’t want people with allergies, and she is now an executive at the Petco Foundation, which supports animal-rescue groups.
One time, the exposure caused an asthma attack so severe that she landed in the hospital for six days.
“If there was a ground zero where someone allergic to cats shouldn’t be, it was my job,” she says. “We were taking in about 20,000 cats a year.”
The hospital stay, however, didn’t dissuade her. Now she swallows Benadryl and other antihistamines before every visit. Afterward, she washes her hands, changes her clothes and takes a shower.
Ms. Cosby, who resides in San Antonio, also adopted a feral cat that was about to be euthanized. The arrangement worked perfectly.
She couldn’t touch the cat, and the cat, named Milkshake, couldn’t stand being touched. He lived with her for 12 years. “I would play with him using feather toys,” she says.
Alia Malik, a 32-year-old journalist who also lives in San Antonio, says a recent allergy test confirmed her suspicion that she has been allergic to cats for several years.

But when the doctor suggested she keep her gray tabby, Sol, off the bed, she refused. “Nothing is changing about how I deal with my cat—nothing at all,” she says. “She’s very snuggly, and I like to snuggle her.”
Updated: 3-29-2023
Dogs And Cats Linked To Reduced Child Food Allergies
Japanese study tracked pet exposure from prenatal development through early infancy.
Children with dogs and cats in their homes were less likely to develop food allergies than other children, a study published Wednesday shows.
The study, led by Dr. Hisao Okabe of Fukushima Medical University, followed more than 66,000 children who were part of the Japan Environment and Children’s Study.
Analyzing questionnaires, researchers tracked pet exposure from prenatal development through early infancy, and measured the incidence of allergies in children up to 3 years old.
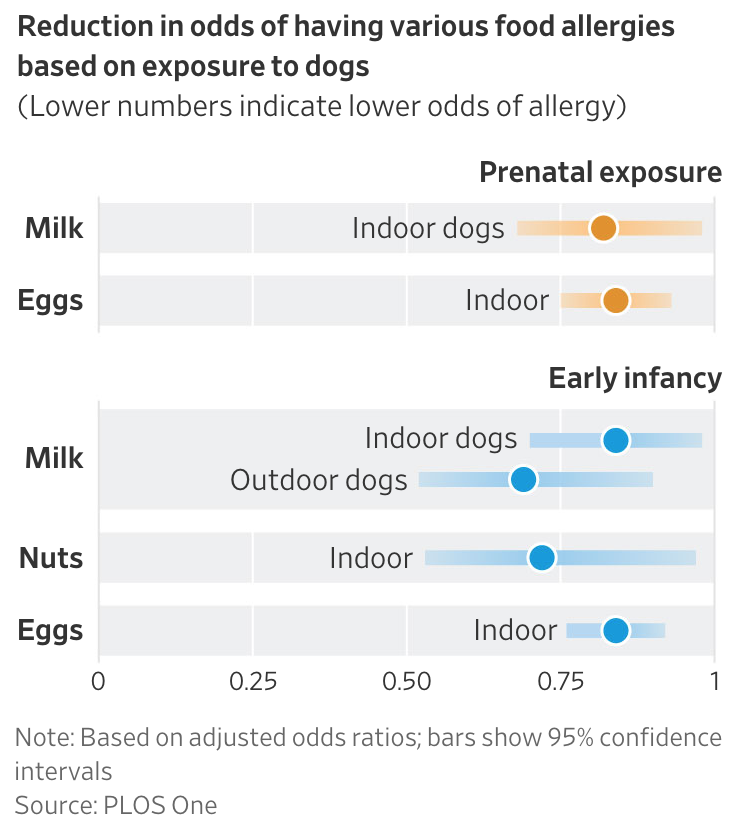
They found that children living with indoor dogs were less likely to experience egg, milk and nut allergies.
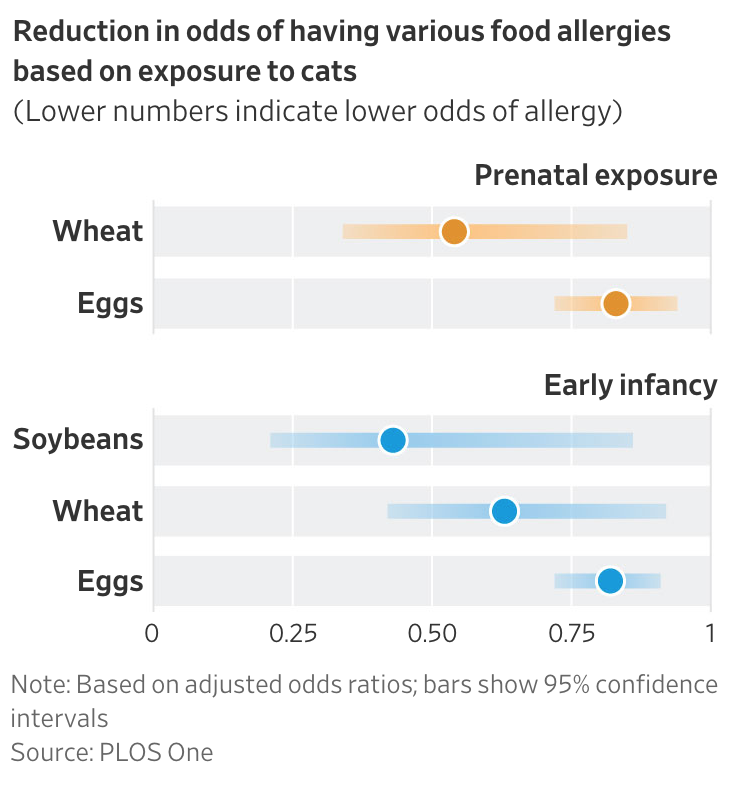
They also determined that children with cats were less likely to have egg, wheat and soybean allergies.
In general, children exposed to pets during both prenatal development and early infancy had lower rates of food allergies than those exposed in only one of these stages. And children living with dogs allowed indoors had lower allergy rates than those with dogs who live outdoors.
The study found that fish, fruit, crustacean and buckwheat noodle allergies weren’t significantly associated with exposure to pets. Other pets, such as turtles or birds, had no significant association with food allergies. Hamsters, however, were associated with an increased incidence of nut allergies.
The study, published in the Journal PLOS One, builds on previous research, including a recent South African study that found exposure to farm animals during fetal development or infancy decreased the risk of food and other allergies.
The current study is unique in its large sample size, range of pets and foods examined, and in its differentiation between prenatal and postnatal exposure, according to the authors.
Food allergies affect more than 5% of U.S. children, according to the U.S. Centers for Disease Control and Prevention. They can have serious, sometimes life-threatening, consequences.
In explaining why pet exposure may affect food allergies, the researchers pointed to the so-called hygiene hypothesis, which says that contact with bacteria and other microbes, including from animals, may be essential for building a healthy immune system.
Having pets in the house might inoculate the GI tract of babies and lead to a more tolerant immune response that is less sensitive to allergens, some researchers have suggested.
“Pet exposure may increase abundance of certain gut microbes as well as contribute to the diversity of gut bacteria, which is possibly associated with lower rates of allergic disease,” Dr. Okabe said.
Dr. Edwin Kim, chief of Pediatric Allergy-Immunology at University of North Carolina School of Medicine, noted that food-allergy rates are higher in the developed world, where disinfectants and other modern conveniences may limit our exposure to microbes.
“Are we too clean, not challenging our immune systems the way they should be?” he asked.
The authors noted several caveats to the study, including that they didn’t test children directly for allergies, but rather relied on doctors’ diagnoses reported by parents.
Dr. Kim, who wasn’t involved in the research, praised the study’s large sample size but noted its subjects were limited to Japan, whose unique genetic or environmental characteristics might not apply to other countries.
A new, large-scale National Institutes of Health-sponsored U.S. birth cohort study called Sunbeam, which is examining early risk factors for allergies including environmental exposures, may provide results that confirm and expand on the current study, he said.
Related Articles:
There Is Now Scientific Proof Your Cat Is Ignoring You (#GotBitcoin?)
My Cat Allergy Is Killing Me, But Cupcake Stays (#GotBitcoin?)
Cat Communication And Healing- The Enigmatic Purr (#GotBitcoin?)
Animal Legal Defense Fund (Animal Rights vs And Animal Welfare)
Meet The Scientists Bringing Extinct Species Back From The Dead (#GotBitcoin?)
Our Facebook Page
Your Questions And Comments Are Greatly Appreciated.
Monty H. & Carolyn A.
Go back
Leave a Reply
You must be logged in to post a comment.