Opiate-Addicted Babies Are The New Crack Babies of 2020
Hospitals around the country are confronting an unsettling consequence of the prescription-pain-pill epidemic: a surge in the number of babies born dependent on drugs such as oxycodone.
Hospitals in Florida and elsewhere are grappling with the latest fallout from the epidemic of prescription-drug abuse: babies born addicted to painkillers. The newborns present new challenges for hospitals.
One recent morning a 12-day-old girl lay writhing in the neonatal intensive-care unit at Sarasota Memorial Hospital . Erin Weatherwax , a nurse, tried to console the newborn by holding her against her chest and patting the baby’s back. She placed the girl in a motorized swing that made cricket sounds. But the infant continued to squirm, unable to sleep more than a few minutes at a time.
The baby suffered withdrawal from methadone, a drug used to treat painkiller addiction that her mother took during pregnancy. The hospital sated the baby’s physical cravings by giving her morphine as well as phenobarbital, a barbiturate used to treat seizures. Now she had to be weaned off those drugs.
Born Dependent on Opioids

Eight hours after Gabriel was born, he exhibited a variety of withdrawal symptoms, including stiffened muscles and excessive sucking.
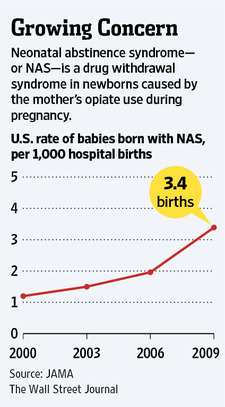
“It’s heartbreaking,” Ms. Weatherwax said. Between 2000 and 2009, the number of newborns showing symptoms of withdrawal from drugs called opioids–including painkillers like oxycodone and anti – addiction drugs such as methadone–tripled in the U.S., according to a study published earlier this year in the Journal of the American Medical Association.
In 2009, more than 13,000 babies in the U.S. were diagnosed with the condition, formally known as neonatal abstinence syndrome , the study said.
The newborns–reminiscent of the “crack babies” of the 1980s and 1990s born to women addicted to cocaine–present a host of challenges to hospitals. There is no standard way to treat their withdrawal, so doctors and nurses are improvising to figure out the most effective combination of drugs and dosages.
The babies require constant attention, and their stays in a neonatal intensive care unit, or NICU, can stretch for weeks, tying up hospital resources. Their treatment is costly–a mean of $53,400–according to the JAMA study, and Medicaid covers the tab for 78% of the babies. Hospital charges to care for such infants jumped to an estimated $720 million in 2009 from $190 million in 2000, the study said.
Hospitals in states such as Kentucky and West Virginia have reported a sharp rise in the number of opioid-dependent babies. In Florida, long the nation’s epicenter of illegal prescription-drug sales, the problem is acute, especially in a cluster of counties near Tampa Bay, including Sarasota. Hospitals such as Spring Hill Regional Hospital, north of Tampa, said that as many as 30% of the babies in their NICUs suffer from opioid withdrawal.
Hospitals were ill-prepared for the drug-dependent infants. “This isn’t a problem I learned about in training,” said Terri Ashmeade, medical director of the NICU and chief of pediatrics at Tampa General Hospital. Her unit, like others, relied at first on protocols for heroin withdrawal in babies, mainly using phenobarbital, she said. But the staff quickly found that withdrawal symptoms for today’s painkillers, which are powerful and long-acting, were much more severe.
The newborns cry incessantly, jerk their limbs and vomit. They can have such severe diarrhea that it burns the skin off their bottoms. Though treating them with the very opioids they are withdrawing from may seem jarring, doctors say the alternative could be worse: seizures and even death.
After years of trying different treatments, Tampa General settled on a uniform approach three months ago. Like many hospitals, it relies on a system that assigns points for different symptoms, and it initiates drug treatment if the numbers cross a certain threshold. (There is no blood test or other diagnostic to determine whether a baby is drug-dependent.)
Eight hours after he was born, Gabriel, a baby undergoing treatment recently at Tampa General’s NICU, exhibited a variety of symptoms, including stiffened muscles and excessive sucking. So the hospital gave him methadone and, when the symptoms persisted, increased the doses until he reached the maximum. Two days later, he was still scoring high, so the hospital gave him clonidine, a drug used to treat withdrawal in adults.
At eight days, Gabriel was still taking the maximum dosage of methadone and close to the maximum of clonidine. He appeared mostly calm, but startled and trembled at times. It would likely take weeks more to wean him off the drugs, nurses said.
Sixty miles to the south, Sarasota Memorial is following a different protocol. While using the same scoring system, it starts babies on morphine, and if necessary, adds phenobarbital.
Hospitals have no choice but to experiment, given the paucity of research on what treatments are most effective. The American Academy of Pediatrics in February published new guidelines for neonatal abstinence syndrome–its first update since 1998. Though the paper cited a range of potential treatments, it didn’t recommend one particular protocol.
To try to come up with a standard regimen, a collaborative of Florida hospitals, including Sarasota Memorial, plans to compare various approaches. Each NICU will rely on morphine and clonidine, but at different dosages, increased and decreased at different rates, said Mark Hudak , a neonatologist at Wolfson Children’s Hospital in Jacksonville, which is part of the group. The group hopes to assemble its findings some time next year.
One objective is to cut down the amount of time babies are spending in intensive care and assess whether they are being over – medicated, Mr. Hudak said.
Hospitals are grappling with another concern: They worry they aren’t catching all the affected babies. Not every mother is forthcoming about using prescription painkillers, which leaves it up to medical staff to look out for symptoms. Most newborns are discharged within 48 to 72 hours, yet babies exposed to long-acting opioids like methadone can take five or more days to show signs of withdrawal.
“Some are going home and withdrawing,” said Tony Napolitano , medical director at Sarasota Memorial. And a mother with dependency issues may not be equipped to handle a highly irritable and sensitive newborn, he said.
Organizations like the Healthy Start Coalition of Hillsborough County, a nonprofit, are urging obstetricians to broach the subject of opioid use with their patients. Many don’t, often because they are unaware how widespread the problem is, said Executive Director Jane Murphy.
Because the phenomenon of opioid-exposed babies is so new, little is known about any long-term effects. Some studies suggest they are at greater risk of attention deficit hyperactivity disorder, but the findings aren’t conclusive.
Fears that the “crack babies” of decades past would develop severe physical, mental and emotional disabilities proved to be unfounded, research showed. But prescription-drug exposure ” seems to be affecting babies’ physiologies more than cocaine,” said Ms. Ashmeade, the Tampa General neonatologist.
What Do You Get When Legal Drug Dealers Peddle “Heroin-in-a-Pill” to it’s “Clientele”?
Jaclyn Kinkade , a 23-year-old doctor’s-office receptionist and occasional model, was a casualty of America’s No. 1 drug menace when she overdosed and died, alone, in a tumbledown clapboard house in Dunnellon, Fla.
The drugs that killed her didn’t come from the Colombian jungles or an Afghan poppy field. Two of the three drugs found in her system were sold to Ms. Kinkade, legally, at Walgreen Co. and CVS Caremark shops, the two biggest U.S. pharmacies. Both prescription drugs found in her body were made in the U.S.–the oxycodone in Elizabeth, N.J., by a company being acquired by generic-drug giant Watson Pharmaceuticals Inc., and the methadone in Hobart, N.Y., by Covidien Ltd., another major manufacturer. Every stage of their distribution was government-regulated. In addition, Ms. Kinkade had small amounts of methamphetamine in her system when she died.
The U.S. spends about $15 billion a year fighting illegal drugs, often on foreign soil. But America’s deadliest drug epidemic begins and ends at home . More than 15,000 Americans now die annually after overdosing on prescription painkillers called opioids, according to the Centers for Disease Control and Prevention–more than from heroin, cocaine and all other illegal drugs combined.
Rising opioid abuse means that drug overdoses are now the single largest cause of accidental death in America. They surpassed traffic accidents in 2009, the most recent CDC data available.
Paradoxically, the legality of prescription painkillers makes their abuse harder to tackle. There is no Pablo Escobar to capture or kill. Authorities must contend with an influential lobby of industry representatives and doctors who argue against more restrictions, saying they would harm legitimate patients. And lawmakers have been reluctant to have the federal government track Americans’ prescriptions, leaving states to piece together a patchy, fragmented response.
Ms. Kinkade’s final days, and the path of the drugs that killed her, were reconstructed from medical and prescription records, police files and interviews. Many records were assembled by Ms. Kinkade’s father and stepmother.
Shuffling through the documents at their living-room table, Bruce Kinkade, a garage-door salesman, and his wife, Ann, said they don’t wish to absolve their daughter of responsibility. “We’re not naive and want to say she was a perfect angel,” said Ann Kinkade, Jaclyn’s stepmother.
Tracing the Path of Prescription Painkillers
Jaclyn Kinkade: A Family Photo of Jaclyn Kinkade As a Child With a Composite of The Prescription Records.
But the Kinkades say the companies and licensed professionals that supplied her with the drugs must also bear some responsibility. “Jackie didn’t wake up one day and say, ‘Hey, I’m going to be a drug addict today,'” Ann Kinkade said. “Jackie pretty much got sent there by a doctor, got hooked and continued to go back.”
There are few easy villains in prescription drug abuse. Companies, physicians and addicts alike are all pieces in a complex puzzle. For some time, regulators have been cracking down on doctors who prescribe to addicts for profit. Now, federal and state officials are starting to move up the supply chain to pursue pharmacies and distributors.
On Sept. 12, the Drug Enforcement Administration revoked the licenses of two Florida CVS stores, which it claims sold excessive amounts of oxycodone without ensuring the pills weren’t diverted to the black market. CVS is fighting the DEA’s order in administrative and federal courts.
Two days later, the agency served Walgreen with a suspension order halting sales of controlled substances from its Jupiter, Fla., distribution center, calling it an “imminent threat to public safety.” The DEA’s regulatory action alleges that the facility–the state’s largest oxycodone distributor–” failed to maintain effective controls ” of its narcotic painkillers.
Walgreen said it is working with regulators and has tightened its procedures. CVS said it was committed to working with regulators “to reduce prescription drug abuse and diversion while ensuring access to appropriate, effective pain medication for our patients who need them.”
Participants in the drug-supply chain acknowledge the problems but point to others as the weak link. Doctors involved say pharmacies should be able to tell if patients are secretly using several physicians to obtain more drugs. Druggists say they can’t second-guess a valid prescription. Manufacturers and distributors say they are simply delivering products ordered by health-care professionals.
What makes this drug scourge different from previous ones, such as heroin in the 1970s and cocaine in the 1980s, is that everyone in the distribution chain is identifiable . The DEA itself controls the supply spigot by setting drug companies’ production quotas for opioids like oxycodone and hydrocodone.

For years, opioids were reserved mainly for cancer or terminally ill patients because of fears over their safety and addictiveness. But over the past 15 years, many doctors have come to view them as an essential tool to manage chronic pain. Around the same time, drug makers began marketing patented, time-release formulations of the drugs, making it a lucrative category.
Today, a growing number of doctors say the pendulum has swung too far, with powerful narcotics being dispensed for even relatively minor complaints. Last year, pharmacies dispensed more than $9 billion in prescription opioid painkillers, more than twice the amount a decade earlier, according to IMS Health, a research firm. The number of prescriptions has risen fourfold. The generic version of Vicodin, a blend of hydrocodone and acetaminophen, is now the most prescribed drug in the country.
Opioids come from the same narcotics family as heroin and can produce similar addictions, researchers say. “We’re basically talking about heroin pills,” said Andrew Kolodny, chairman of the psychiatry department at Maimonides Medical Center in New York.
Studies show that opioid addicts come from a surprisingly broad swath of the population: the middle-age, the elderly and, increasingly, young adults. Many U.S. veterans returning from Iraq and Afghanistan with physical and mental injuries are also becoming dependent on prescription painkillers, researchers say.
In recent decades, researchers have come to view addiction as a disease, rather than just a personal failing. Some people are more predisposed to becoming addicted because of heredity, experience and other factors that have yet to be fully understood. But some drugs are simply more addictive than others.

Jaclyn Kinkade Before She Began Taking Drugs.
New research suggests that drugs like opioids cause long-lasting changes to the brain, rewiring some areas to crave more drugs while simultaneously damaging the parts that can control those cravings. The drugs can damage the brain’s ability to feel pleasure, so regular users eventually need to take them not to get high or help with pain, but just to feel normal. Avoiding unpleasant withdrawal symptoms end up conditioning many drug users’ daily lives.
One of the most confounding aspects of this latest epidemic is that it blurs the lines between legal and illegal drug use. Some people first take drugs from their family medicine cabinets to get high, then go to doctors to get more. Others are originally prescribed the pills for legitimate reasons, then buy them on the street once they’re hooked.
Many, such as Ms. Kinkade, end up mixing legal and illegal drugs in ways that can prove lethal.
Ms. Kinkade was a lively, talkative woman with blond hair, a fear of caterpillars and a pit-bull terrier, Bentley, that traveled everywhere with her.
She was first prescribed an opioid on Oct. 27, 2006, by the doctor who employed her as a receptionist, prescription records show. According to medical records and an entry from her diary, she had been suffering back and neck pain. Thomas Suits, her employer, prescribed 20 pills of Endocet, a drug containing oxycodone. “I’d never taken opioids before,” Ms. Kinkade wrote in a diary entry. “But I started the med routine and OMG I felt no pain.”

Jaclyn Kinkade On Vacation When She Was 21 Years Old. She Died Of An Accidental Drug Overdose About Two Years Later, At Age 23.
Dr. Suits didn’t recall prescribing the medication, said his wife, Irene Machel, a doctor who also works at the clinic. She declined to discuss the matter further.
Endo Health Solutions, which made the pills, declined to comment on Ms. Kinkade . “These types of stories are tragic and we obviously take them seriously,” said Endo spokesman Blaine Davis. “Our responsibility, as a company that is very dedicated to the field of pain management, is to educate both physicians and patients about appropriate use.”
Soon Ms. Kinkade was seeking more drugs. On Jan. 5, 2007, she saw Bruce Kammerman, a family practitioner at a clinic in Stuart, Fla., and came away with a generic blend of oxycodone and acetaminophen. A scan taken a month later showed no problems with her spine, according to the medical report. Through his lawyer, Dr. Kammerman declined to say why he wrote the prescription. “That’s a sad case,” said his attorney, Lance Richard. “Maybe she didn’t have justifiable pain but she certainly came in and made complaints about it. At some point the doctor just has to go on the patient’s word.”
Dr. Kammerman was arrested in July at a pain clinic in Vero Beach, Fla., charged with drug trafficking, racketeering and illegally selling controlled substances. The DEA said in a news conference he was prescribing an average of 1,700 oxycodone tablets a day. Dr. Kammerman’s lawyer said his client has done nothing wrong and pleaded not guilty.

Jaclyn Kinkade In a Mug Shot on May 10, 2010, Two Months Before Her Death.
Ms. Kinkade broke up with her boyfriend. She began missing work. One day she was found curled up under her desk, crying. “She always used to be clean-cut, nice makeup,” said Susan Cochran, a former colleague. Then “she would come in in sweatpants and it was like: ‘Who is this person?'”
Ms. Kinkade changed jobs to work at a radiologist’s office. There, she had two other scans, in April and July 2008. Neither showed significant spine problems, according to the medical reports. Ms. Kinkade started seeking clinics that asked fewer questions. ” Family practitioners hate writing narcotics ,” she wrote in her diary. “Nowadays–I’ll just go str8 to pain docs.”
During that period, she was prescribed large amounts of oxycodone, her records show, combined with anti-anxiety drugs and powerful muscle relaxants. Her parents grew increasingly alarmed. “Sometimes you’d be having a conversation with her and her head would just drop,” Mr. Kinkade said. “And she’d say: ‘Oh, I’m just tired; I was out late.'”
After reviewing her records, he said, “We estimated that at one point she was taking 13.4 pills per day, for nothing wrong with her.”
In May 2009, Mr. Kinkade and his wife asked a judge to have their daughter forcibly admitted to drug treatment under a Florida law. Their request was initially denied because she wasn’t a minor. Angered by their efforts, Ms. Kinkade moved out of their home and drove across the state to her biological mother’s house. She crashed her car and was found wandering along the highway in a drug-induced daze, her parents said, searching for her pills.
Legal records show she was arrested several times for minor crimes such as possessing controlled drugs without a prescription and shoplifting small items, including makeup and cake topping. In each case, she was released and the charges dropped.

She started visiting a pain clinic in Tampa called Doctors Rx Us , where she was prescribed oxycodone, methadone, alprazolam and gabapentin, an antiseizure medication, according to records her parents collected. Housed in a rundown strip mall, the clinic today is called Palm Medical Group after a name change in 2011, according to its state records.
Ms. Kinkade was prescribed the drugs by two physicians at Doctors Rx Us: Richard Smith and William Crumbley. Dr. Crumbley was arrested in December and charged with operating a nonregistered pain clinic at another location. He has pleaded not guilty.
Dr. Smith and the clinic declined repeated interview requests. A lawyer for Dr. Crumbley said he was innocent of any wrongdoing.
On May 3, 2010, Ms. Kinkade stopped at a CVS in Crystal River, Fla., and picked up a prescription written by Dr. Smith for 90 tablets of 10mg methadone, along with 90 tablets of alprazolam, an antianxiety drug.
“Jaclyn Kinkade’s death is a terrible tragedy that highlights the need for a comprehensive national effort to prevent prescription drug abuse,” CVS said in a statement.
Information provided by the manufacturer suggests that the methadone dispensed to Ms. Kinkade was likely supplied to CVS by Cardinal Health Inc. Cardinal was the only distributor to have sold that particular drug to that CVS branch during that period, according to the manufacturer’s records. CVS and Cardinal declined to comment.
Last year, the DEA launched a probe of the Florida-based operations of Cardinal Health and CVS Caremark. The agency alleged they dispensed “extremely large amounts” of oxycodone with signs that the drugs were “diverted from legitimate channels.”
CVS said it has “responded to the DEA’s concerns, including implementing enhancements to our policies and procedures for filling controlled substance prescriptions.” Cardinal settled with the DEA in May, agreeing to suspend sales for two years at one of its key distribution facilities in Lakeland, Fla.
The methadone Ms. Kinkade picked up at the end of her life was made in Hobart, N.Y., by Mallinckrodt , a unit of health-care giant Covidien . “Any death from abuse or misuse of prescription drugs is tragic,” Covidien said. “That’s why we believe that, as a nation, ending the abuse, diversion and misuse of powerful pain medications is necessary to ensure adequate treatment of pain and access to that treatment for legitimate pain patients.”
On May 10, 2010, Ms. Kinkade was stopped by police in Levy County, Fla., for having an expired registration. A drug-sniffing dog reacted to her car and she was arrested for possessing a generic form of Xanax without the correct prescription. This time, her parents let her sit in jail for a couple of weeks while they organized a place for her in a rehabilitation program. They bailed her out May 25 and enrolled her in drug treatment.
Over the next month, Ms. Kinkade went to the treatment program during the day and seemed to improve, her parents said. Then, the evening of June 24, she climbed out the window at her parents’ house.
A few days later, on the other side of Florida, she met up with a boyfriend, according to a statement he later gave police. She returned to Doctors Rx Us, where Dr. Smith wrote a prescription for 90 tablets of 30mg oxycodone, according to prescription records. It would be her last.
The next day, Ms. Kinkade filled the prescription at a Walgreens in Beverly Hills, Fla. The oxycodone would have come from Walgreen’s Jupiter, Fla. , distribution center, a company spokesman said. On Sept. 14, the DEA barred that facility from selling controlled substances, alleging that it failed to maintain effective controls to stop large amounts of oxycodone from reaching the black market. “When [companies] choose to look the other way, patients suffer and drug dealers prosper,” Mark Trouville, the DEA special agent in charge, said at the time. Walgreen said in a statement it is cooperating with the DEA.
The oxycodone came from the New Jersey plant of Actavis, a Swiss pharmaceutical company. In April, Actavis was bought by Watson Pharmaceutical in a $5.8 billion deal awaiting regulatory approval. An Actavis spokesman described Ms. Kinkade’s situation as a “tragic occurrence” and called for discussion on “how to prevent such cases in the future.” A Watson spokesman cautioned against action that would make it harder to treat legitimate patients . He said the company supported educating patients about the drugs’ proper use.
The morning of July 4, Ms. Kinkade’s boyfriend found her sitting cross-legged and slumped in his room at a white, low-slung house tucked behind a trailer park. The medical examiner said she died from a drug cocktail including oxycodone, methadone and methamphetamine.
Ms. Kinkade’s physical decline made such an impression on the detective who investigated the case that, two years later, he still recalls the scene. In the living room, he noticed a poster of Ms. Kinkade modeling for a biker magazine.
“Wow, she’s a beautiful young lady,” Detective Matthew Taylor remembered thinking. “When I actually saw her, it was as different as night and day.”
Related Articles:
Freedom of Information Act Document Reveals Antidepressant Drugs Are Less Effective Than Placebos
Fentanyl’s New Foe: A Quick Test Strip That Can Prevent Overdoses (#GotBitcoin?)
Pharmaceuticals Found In Our Drinking Water!
What Do You Get When Legal Drug Dealers Peddle “Heroin-in-a-Pill” To It’s “Clientele”?
Your questions and comments are greatly appreciated.
Monty H. & Carolyn A.
Go back
Leave a Reply
You must be logged in to post a comment.